OASIS HOSPITAL SOLUTIONS
India’s 1st Award-Winning Claim Assistance Company
Looking for One Stop Solutions of Hospitals for Health Insurance Services.
ABOUT US
Having a wide range of experience in, Claims procedure, Health Government Projects/ Scheme Tie-up with Insurance Co, and Marketing. We have started to provide services to the Hospital Industry.
PAN India NABH Consultation and Surveillance services are just a call away.
Since then, we’ve processed thousands of claims, growing with our market through years of expansion and regulatory changes. We’ve met those challenges with new services, technologies, and acquisitions to develop an infrastructure for serving our customers in an ever-evolving healthcare environment


NABH
- NABH (National Accreditation Board for Hospitals & Healthcare Providers) is an organization in India that sets standards for quality healthcare services in various healthcare settings such as hospitals, clinics, and nursing homes. NABH accreditation is the recognition that a healthcare facility has met these quality standards and is committed to providing safe, effective, and patient-centered care.
- A NABH consultant is a professional who provides guidance and assistance to healthcare facilities seeking NABH accreditation. Their role is to help healthcare facilities understand the NABH standards and requirements, assess their current practices and procedures, identify areas for improvement, and develop and implement a plan to meet the NABH standards.
TPA Desk Management
- Supervising and managing a team of claims processors and administrators to ensure timely and accurate processing of health insurance claims.
- Reviewing and verifying the accuracy and completeness of claim submissions, including medical records, bills, and other supporting documents.
- Adjudicating claims by established policies and procedures, ensuring compliance with regulatory requirements and contractual obligations.
- Negotiating with healthcare providers to resolve disputed claims, including fees and reimbursement amounts.
- Analyzing claim data and identifying trends or patterns that may indicate fraudulent or abusive billing practices.
- Developing and implementing strategies to improve claims processing efficiency and accuracy, and reduce claims costs.
- Collaborating with other departments, such as customer service, network management, and medical management, to ensure seamless and coordinated delivery of health benefits to members.

Corporate, Insurance & TPA Business Company Tie up
- Corporate and third-Party Administrator (TPA) tie-ups important for hospitals to increase their patient base, revenue, and brand image.
- Insurance Companies
- Third-Party Administrators (TPAs)
- Government Project PMJAY
- Governmental agencies like ECHS, CGHS, DGEHS, MCD, DDA & others
- Corporate tie-ups for health check-ups
- The practice/health care set empanelled with this network provides cashless or charges a minimum to avail of diagnostic services or hospitalization by them.
Tie with up Services with Government Yojana
- To tie up services with an insurance company, you would typically need to establish a partnership or contractual agreement between your company and the insurance provider. The exact details and requirements may vary depending on the specific insurance company and the type of services you offer. However, here is a general outline of the steps involved:

Benefit to Hospitals
- Cashless processing eliminates the need for manual cash handling and associated administrative tasks, such as counting, reconciling, and depositing cash. This leads to increased operational efficiency, as hospital staff can focus on core responsibilities instead of cash management.
- Handling cash involves various costs, including cashiers’ wages, secure storage facilities, armored transportation, and the risk of theft or loss. By adopting cashless processing, hospitals can reduce or eliminate these expenses, resulting in significant cost savings over time.
Medi Claim Bill Review Systems
- Healthcare Industry Medical Bill Review Systems services involve the evaluation and analysis of medical bills to ensure accuracy, appropriateness, and compliance with regulations. These systems play a crucial role in reducing healthcare costs, minimizing billing errors, and optimizing reimbursement processes.
- Overall, Medical Bill Review Systems services are vital in the healthcare
industry to ensure accurate billing, optimize reimbursements, and control costs. They contribute to improved financial outcomes, regulatory compliance, and enhanced patient care by minimizing billing errors, detecting fraud, and providing valuable insights for decision-making.

Medical Claims Processing Streamlined for Quick Results
- Medical Billing Experts has been helping healthcare providers increase revenue by organizing their medical claims processes. Our strength lies in our commitment to accuracy, efficiency and flexibility, which we incorporate across the entire gamut of healthcare claims processing service.
- We have developed a robust model for managing claims operations for our clients. These models have evolved through our decade long experience in claims processing and offer our clients the most optimal way to process claims. Some of these models are based on categories of rejected claims, created by special teams assigned with the task of monitoring, understanding and pursuing rejected claims.
- We also provide our clients with complete control over rejected claims. As one of the leading medical claims processing companies in the industry, our clients can check how the claim is progressing in real time and analyze the efficiency of the various stages of the medical claims management process.
Root Cause Analysis ( RCA)
- Root Cause Analysis (RCA) is a systematic approach used in the healthcare industry to identify and understand the underlying causes of adverse events, medical errors, or near-misses. It aims to uncover the factors and processes that contribute to these incidents, to prevent their recurrence and improve patient safety.
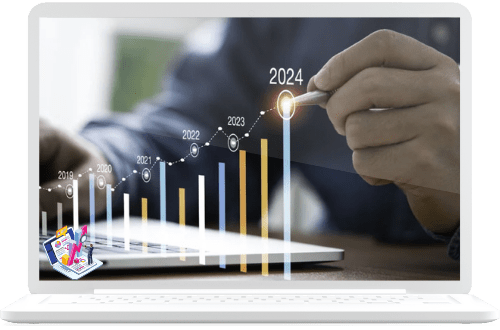
Best Healthcare Services Awarded By Gujarat Health Minister.
ISO: 9001 - Certified Company
PAN India Service provider
50+ Crore Amount Claimed Yearly
2,75,000+ Claims Processed
1000+ hospitals Successfully Meeting across India
Associate with 300+ Hospitals
500+ Projects Done
"I attribute my ability to achieve goals and provide quality services to Oasis. Oasis is an honest, ethical, and transparent organization that consistently provides knowledge and technology. The user-friendly web portal serves as a 'one-stop solution' for all my needs. Thanks to the CMS team for their wonderful support."
100-Beds Hospital"I've awarded Oasis a 5-star rating for their exceptional service in managing cashless empanelment and processing at my hospital. They have demonstrated their capability in achieving hospital goals and ensuring a smooth working environment for our doctors. Now, our doctors prefer cashless patients at our hospital exclusively."
200-Beds HospitalCareer Opportunities
Oasis Hospital Solutions Team Has 27+ Years of experience, All Management Team Members Are Industry Experts.

Mr. Rahul Shah
Board Member

Mr. Ravi Waghmare
Zonal Head - Operation

Mr. Ravinder Singh
Marketing Head

Ms. S Shaikh
Operation Head

Ms. Yumna
Claims Head

Mr. Rahul Shah
Board Member
Excellence Award from the Gujarat Health Minister

Business Locations

